- +91 8591314766
- info@smaarogya.com
AarogyaDaan - Our Social Impact Initiative
Why should you support AarogyaDaan?
- Promote Disease Prevention
- Improve Primary Healthcare Delivery
- Help the Vulnerable and Needy
Let's join hands to make India healthier
- Help us to give the Preventive Healthcare Shield to the needy and vulnerable, free or at a subsidized rate.
- Help us leverage our data analytics and healthcare expertise, to collaborate with all Stakeholders to plan better primary infrastructure and ensure optimal resource management.
- Become empowered – we provide a transparent way of donating – monitor and assess outcomes for your efforts with our dashboards and reports.
How will Preventive Healthcare Benefit India?

It will lead to prevention and early treatment.

It will increase health education and awareness.

It will lead to targeted health intervention.

It will improve public health planning.

It will enable evidence-based policy making.

It will ensure effective resource allocation.

It will promote and ensure health equity.

It will foster stakeholder collaboration.
BalAarogya - A School Health Program
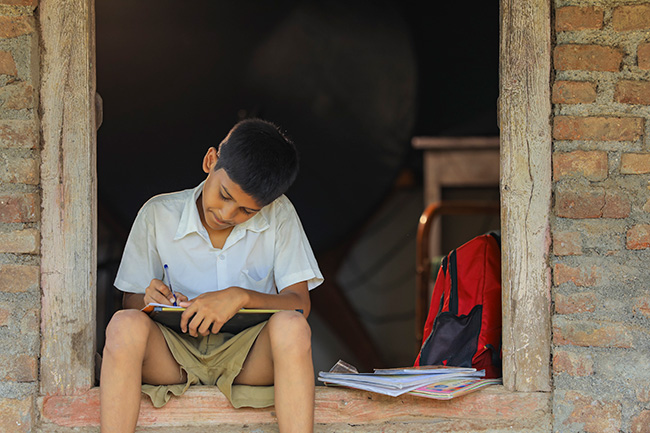

Healthy kids,
improved learning...
BalAarogya conducts a health risk assessment survey and an annual health program for students in municipal/government-run schools and aided schools that cater to the lower middle and poorer socio-economic strata of society.
TAX BENIFIT / CSR CERTIFICATE AVIALABLE
Project Thrive
10,000 students
BMC Schools
Location Govandi & Chembur Mumbai
Amount to be raised – Rs 2.00 Crore
Minimum Contribution – Rs 20 Lac
(Cost per school)
Our NGO Partner
Ravindra Joshi Medical Foundation
TAX BENIFIT / CSR CERTIFICATE AVIALABLE
Project Padma
1600 students
Kumud vidyamandir
Location Govandi (East), Mumbai
Amount to be Raised – Rs 32.00 Lac
Minimum Contribution – Rs 2 Lac
(Cost per 100 students)
Our NGO Partner
Ganga Charitable Trust
Are you passionate about making a difference? Support this cause. We invite you to explore the project brochure and additional details, which provide comprehensive information about our initiatives and the positive impact we aim to create.
Our current social initiatives
Promoting community health: Empowering villages in Mumbai through Health Risk Assessment
We are pleased to announce our collaboration with SAVALI Foundation, an esteemed NGO, to conduct a comprehensive Health Risk Assessment survey in the villages of Mahul, Mahul-SRA, Ambapada, Gawanpada, and Vishnunagar in Mumbai. We aim to reach as many individuals as possible in these villages. The population residing is approximately 25,000. This significant initiative is valued at Rs 23.25 Lac and has received generous support from our esteemed corporate partner, BPCL.
The primary objective of this survey is to assess the health risks and needs of the community members in these villages. By collecting valuable data and insights, we aim to identify potential health concerns, establish targeted interventions, and promote preventive healthcare practices.
Our past social initiatives
Empowering Communities: Health Awareness and Prevention
Previous
Next
At Smaarogya, we remain dedicated to creating impactful social initiatives and making a positive difference in communities. Stay tuned for our upcoming projects and opportunities to contribute to building a healthier and more inclusive society.
Frequently Asked Questions
General
Building a Healthier Future: Empowering Communities through Preventive Healthcare and Collaborative Planning
We are dedicated to extending the reach of preventive healthcare to vulnerable populations, including underserved communities, rural areas, and socioeconomically disadvantaged groups who often face barriers to accessing healthcare services. Our goal is to address health inequities, improve health outcomes, and foster inclusivity in healthcare through targeted health risk assessments, screenings, and interventions.
1. Comprehensive Population Health Surveys:
With your support, we will conduct large-scale health risk assessment surveys to reach a wider population at risk. By gathering valuable data and insights, we can identify prevalent health risks and develop effective strategies for intervention and improvement.
2. Health Screening and Early Detection:
Building on the survey findings, we will organize screening and early detection drives, providing subsidized or free screenings to underserved populations. This proactive approach aims to detect potential health issues at an early stage, allowing for timely intervention and treatment.
3. Health Awareness Campaigns:
In collaboration with you, we will develop educational materials, conduct workshops, and host seminars to raise awareness about preventive healthcare. Empowering individuals with knowledge about health risks, preventive measures, and available resources will encourage informed decision-making and healthier lifestyles.
4. Strengthening Primary Healthcare Delivery:
Utilizing the valuable data and insights generated, we will work towards enhancing primary healthcare delivery. By identifying gaps and areas of improvement, we can guide resource allocation, healthcare planning, and the development of tailored preventive strategies. This collaborative effort will involve healthcare providers, government bodies, NGOs, and community stakeholders, ensuring a comprehensive and community-led approach.
Together, We Can Create a Healthier India.
Join forces with us to shape a healthier India. Let’s come together with a shared commitment to promoting preventive healthcare, emphasizing early detection, and tackling the growing burden of non-communicable diseases (NCDs) and cancers. Through our collective efforts, we have the power to bring about significant change, improving the lives of millions and building a stronger and healthier nation that will thrive for generations.
We extend a warm invitation to you to be a part of our mission to transform the healthcare landscape. By donating to our NGO partners involved in preventive and primary healthcare initiatives, you can make a profound impact. Your generous contribution will not only save lives but also contribute to the creation of a society that is healthier and more resilient. Together, we can forge a future where individuals possess the knowledge, resources, and support necessary to proactively manage their health and well-being.
Addressing the Rising Health Challenges of India: Prioritizing Preventive Health Measures
India is currently grappling with a growing burden of non-communicable diseases (NCDs), including cardiovascular diseases, diabetes, respiratory ailments, and cancers. Factors such as rapid urbanization, sedentary lifestyles, unhealthy diets, and tobacco abuse have contributed to this concerning trend. NCDs and cancers continue to pose significant risks to the well-being and productivity of individuals, families, healthcare systems, and the nation as a whole.
To combat this critical issue, it is imperative to implement population-level health risk assessments and screenings. These initiatives play a vital role in identifying individuals at risk and providing timely interventions. By empowering individuals to make informed decisions about their health, adopt healthier lifestyles, and seek necessary care, population-level assessments serve as powerful tools in the fight against NCDs and cancers. Additionally, regular screenings facilitate the detection of potential abnormalities at early stages, enhancing treatment success rates, reducing costs, and ultimately improving quality of life and productivity.
Key Advantages of Population-Level Health Risk Assessments:
Strengthened Public Health Planning: Population-level assessments offer valuable data and insights into the health risks and requirements of different communities. This information enables the development of effective public health strategies and targeted interventions to address specific health issues. By understanding the health risks at a population level, policymakers can allocate resources and prioritize interventions for maximum impact.
Tailored Health Interventions: Health risk assessments identify vulnerable populations and specific risk factors within communities, enabling healthcare providers, public health agencies, and policymakers to target interventions and resources where they are most needed. For instance, if an assessment reveals high rates of cardiovascular disease, efforts can focus on preventive measures like education campaigns, access to healthy food, and promotion of physical activity.
Promoting Health Equity: Population-level assessments help identify health disparities and inequalities among different demographic groups, guiding efforts to reduce inequities and promote health equity. Tailored interventions addressing the root causes of disparities and ensuring equitable access to healthcare services can be developed based on the specific health risks faced by different communities.
Prevention and Early Intervention: Emphasizing preventive measures and early intervention, population-level assessments aid in reducing the likelihood of disease occurrence or progression. By identifying common risk factors and potential health threats, interventions can be implemented to prevent severe health issues, leading to long-term cost savings and reduced strain on healthcare systems.
Health Education and Awareness: Conducting health risk assessments at a population level creates opportunities for health education and awareness campaigns. Such initiatives raise awareness about prevalent health risks and promote healthier lifestyles within communities. Equipped with information on risk factors, symptoms, and prevention strategies, individuals can make informed decisions about their health, resulting in better overall health outcomes.
Evidence-Based Policy Making: Population-level assessments provide a robust evidence base for policymakers, enabling them to make informed decisions and implement evidence-based policies and interventions. By considering the data gathered from risk assessments, policymakers can effectively allocate resources, prioritize health issues, and monitor the impact of interventions.
Optimal Resource Allocation: Population-level assessments aid in efficiently allocating resources by identifying the most pressing health risks within a population. This information empowers policymakers and healthcare providers to allocate funding, personnel, and infrastructure based on identified risks and priorities. Optimizing the utilization of limited resources through population-level assessments leads to improved healthcare delivery and outcomes.
Fostering Stakeholder Collaboration and Engagement: The process of conducting population-level health risk assessments involves engaging various stakeholders, including community members, healthcare professionals, policymakers, and organizations. This collaborative approach fosters a sense of ownership, inclusivity, and shared responsibility in addressing health risks at the population level. By involving stakeholders, population-level assessments encourage community engagement, empowerment, and participation in decision-making processes related to health. This holistic approach results in the development of sustainable solutions that resonate with the needs and values of the population, ultimately enhancing social cohesion and community well-being.
BalAarogya - A School Health Program
India’s Healthcare Sector is in transition. It is undergoing a major transformation. The burden of non-communicable diseases (NCDs) is increasing, while the share of communicable, maternal, neonatal, and nutritional diseases is decreasing. This is due to several factors, including urbanization, several dietary habits, and an ageing population.
NCDs are chronic diseases that are not contagious. They include heart disease, stroke, cancer, chronic respiratory diseases, and diabetes. These diseases are a major cause of death and disability in India, and they are expected to become even more prevalent in the coming years.
The increasing burden of NCDs is putting a strain on India’s healthcare system. Primary healthcare facilities in urban areas are often inadequate, and they cannot provide comprehensive care for NCDs. This means that people with NCDs often have to travel long distances to access quality care, and they may not be able to afford the cost of treatment.
There is an urgent need to strengthen primary healthcare in urban areas to address the rising burden of NCDs. This will require a multi-pronged approach that includes:
- Investing in the infrastructure and human resources of primary healthcare facilities
- Developing and implementing evidence-based NCD prevention and treatment programs
- Raising awareness about NCDs and the importance of early detection and treatment
The government has a role to play in strengthening primary healthcare, but social impact initiatives can also play a valuable role. These initiatives can help to fill the gaps in care, and they can reach people who are not able to access care through the formal healthcare system.
India is a young country, with more than half of its population under the age of 25. This large youth population is a major asset, and any investment in their education, health, and well-being will have a significant impact on the country’s future.
With so many competing demands for scarce funds, it can be easy to overlook the importance of investing in young people. However, these young people are critical to our national economy, society, and democracy – both today and in the future.
Young people are the future workforce. They are the ones who will be driving innovation and economic growth. They are also the ones who will be shaping our society and democracy.
That’s why it’s so important to invest in programs that support young people. These programs can help young people develop the skills they need to succeed in the workforce, become engaged citizens, and contribute to their communities.
Unfortunately, we are not making adequate investments in these programs. This is a mistake. If we want to ensure a strong future for our country, we need to invest in our young people.
The early years of life are a critical period for human development. During this time, the brain develops rapidly and children acquire essential cognitive, social, and emotional skills. These skills lay the foundation for future success in school, work, and life.
Investing in children and youth is one of the most effective ways to promote socio-economic development. By providing early childhood education, healthcare, and other essential services, we can help children reach their full potential and contribute to a more prosperous society. There are two main reasons why investing in children and youth is so effective:
- The brain develops rapidly during early childhood and adolescence. This means that early investments can have a lasting impact on cognitive development. For example, studies have shown that early childhood education can improve children’s IQ scores and academic achievement.
- Early cognitive and non-cognitive skills and health capabilities lead to enhanced effectiveness of later investment. This means that children who have strong foundational skills are more likely to benefit from later interventions. For example, children who are healthy and well-nourished are more likely to succeed in school.
In conclusion, investing in children and youth is a smart investment for the future. By providing early childhood education, healthcare, and other essential services, we can help children reach their full potential and contribute to a more prosperous society.
We believe that investing in the health of children, adolescents, and youth is essential for the future of our society. The BalAarogya project is a comprehensive program that aims to provide early prevention, assessment, and treatment for health problems in these age groups. We believe that by promoting healthy habits and preventing risky behaviour at an early age, we can help ensure that our future generation is mentally and physically fit.
The health and economic consequences of health risks that develop in early childhood can be very high over the entire lifespan. For example, childhood obesity can lead to chronic diseases such as heart disease, stroke, and diabetes in adulthood. These diseases can result in high healthcare costs and lost productivity. Early intervention can help to mitigate the health risks of early childhood. We often focus on the present and neglect the future. This is why it is important to have effective programs that intervene at a young age to improve the health of school-going children and adolescents. These programs should also aim to reduce inequality, both in terms of gender and socioeconomic status. We believe that this is a societal investment that will benefit both individuals and the entire population.
There are many reasons why investing in children’s health at an early age is a wise strategy. Here are some of the key benefits:
- Long-term benefits: Children who receive proper healthcare and nutrition are more likely to grow up healthy, have better cognitive development, and perform better in school. These benefits can translate into higher earning potential, better job opportunities, and decreased healthcare costs throughout their lives.
- Prevention of chronic diseases: Children who develop unhealthy habits or suffer from chronic illnesses at a young age are more likely to continue these behaviours and suffer from chronic diseases later in life. Investing in children’s health can help prevent these chronic diseases and reduce healthcare costs associated with treating them.
- Economic benefits: A healthy population is essential for economic growth. Healthy children are more likely to attend school regularly and perform better academically, which can lead to higher earning potential and better job opportunities as they enter adulthood. Additionally, investing in children’s health can reduce the burden on the healthcare system and lead to cost savings in the long run.
- Moral obligation: Children are the most vulnerable members of society, and it is our moral obligation to ensure that they have access to quality healthcare and a healthy environment. By investing in children’s health, we are not only helping them lead healthier and happier lives but also fulfilling our responsibility to future generations.
Young people are India’s most precious resource. Almost one-third of India’s population is of school-going age or younger (0 to 18 years). This segment of the population faces many health issues. Some of the key issues faced by them are:
Mental disorders: The prevalence of mental disorders in the age group of 13 to 17 years is 7 per cent. This issue is nearly twice as high in urban areas as in rural areas.
Malnutrition: Malnutrition continues to be a major issue, and micronutrient deficiencies like anaemia (prevalence of around 20 per cent) are rampant in young Indians. Almost ¼ of the children have a BMI lower than BMI-for-age, whereas 5 per cent are overweight.
Tobacco use: About 20 million children ages 10 to 14 years were addicted to tobacco.
Birth defects and developmental delays: 6 per cent of children are born with birth defects, and 10 per cent of children are affected with developmental delays leading to disabilities.
Dental caries: The prevalence of dental caries is more than 50 per cent among Indian schoolchildren.
Rheumatic heart disease: Rheumatic heart disease is reported at 1.5 per thousand among school children aged 5 to 9 years and 0.13 to 1.1 per thousand among 10 to 14 years.
Asthma: The prevalence of reactive airway disease including asthma among children is reported to be around 5 per cent.
Prediabetes and diabetes: 1 in 10 school-aged children and adolescents are prediabetic, whereas 1 per cent are diabetic.
Chronic kidney disease: 7 per cent of school-aged children and adolescents are at risk of developing chronic kidney disease.
Hypertension and high cholesterol: Around 5 per cent of adolescents are likely to have hypertension and around 4 per cent of school-aged children and adolescents are likely to have high cholesterol.
To tackle these issues, active health intervention programs are required to be taken up at the school level. BalAarogya – Building Healthy Communities through Schools is an initiative of Smaarogya to make India “healthier” by implementing a comprehensive Annual School Health Program in Schools.
The program will cover kids in primary, middle, high, and higher secondary schools run by municipal corporations, state governments and trust catering to society’s poor and vulnerable segment. The program intends to ensure equity and fairness by providing quality health interventions to the identified schools, which are generally available to the children of the privileged section of society.
Significant progress has been made in enhancing the well-being of children and adolescents in recent decades. This progress is evident through reduced mortality rates, improved nutrition, and decreased fertility rates among adolescent girls. Despite these achievements, there is still much work to be done. A considerable number of children and adolescents continue to face significant health challenges, which hinder their growth and development to their fullest potential.
The health and safety of school-going children and adolescents are influenced by various internal and external factors. They encounter a range of preventable health issues, including unintentional injuries, interpersonal violence, sexual and reproductive health problems, communicable and non-communicable diseases, mental health disorders, and risky behaviours associated with them, such as tobacco and alcohol use, unhealthy diet, and physical inactivity. Furthermore, children have diverse physical, sexual, psychosocial, and neurocognitive health and developmental needs as they transition from childhood to adulthood.
Early detection plays a crucial role in effectively managing or preventing many of these health conditions. Schools serve as an ideal setting for timely interventions, which include identifying the 4Ds (Defects at birth, Diseases, Deficiencies, and Development Delays, including Disabilities), conducting general check-ups like eye, hearing, and dental screenings, managing anxiety, depression, and behavioural disorders, as well as addressing lifestyle conditions like diabetes, overweight, obesity, and undernutrition.
There is a significant demand for quality healthcare services for 5 to 18-year-olds. However, the quality of healthcare services, particularly in government-run schools and some private schools catering to the underprivileged, varies, and coverage remains limited. Therefore, schools present a unique opportunity to implement effective healthcare services, including preventive measures, on a larger scale for children and adolescents.
Hence, it is essential for the government and all stakeholders involved to prioritize health-related behaviours and conditions, with schools playing a pivotal role in addressing public health challenges. This underscores the significance of BalAarogya – the Annual School Health Program, which takes a comprehensive and holistic approach to young people’s health. The program aims to promote students’ optimal physical, social, emotional, and mental growth by encouraging healthy practices and providing timely medical intervention.
Gaps in School Health Programs: A recent assessment of school health programs in India identified several gaps. These gaps include:
- Lack of provision for first aid: Most schools do not have adequate first aid supplies or training for teachers and students.
- Gender inequity: Many schools lack facilities for adolescent girls, such as sanitary pad dispensers and incinerators. There is also a lack of awareness and education about menstrual hygiene.
- Ineffective distribution of deworming and iron tablets: The distribution of these medicines is often not effective, as it is the responsibility of teachers who are pressed for time.
- Lack of comprehensive health assessments: Most schools do not conduct comprehensive physical and mental health assessments.
- Inadequate prevention of tobacco/alcohol and other substance abuse: There is a lack of awareness about the harmful effects of substance abuse, especially among adolescent students.
- Lack of preventive health education: Most schools do not provide health education workshops or awareness campaigns for disease prevention.
- Lack of sporting facilities: Many schools lack sufficient sporting infrastructure in terms of space and equipment.
- Lack of mental health programs: Almost no school has any program for tackling students’ mental health issues.
- Ineffective health check-up camps: Health check-up camps are often conducted in a random and unplanned manner.
- Lack of student health records: Most schools do not have or maintain student health records.
Recommendations: The following recommendations are made to address the gaps in school health programs:
- Provide first aid supplies and training to teachers and students.
- Provide sanitary pad dispensers and incinerators for adolescent girls.
- Centralize the distribution of deworming and iron tablets.
- Provide safe drinking water and sanitation facilities in all schools.
- Conduct comprehensive physical and mental health assessments for all students.
- Educate students about the harmful effects of tobacco/alcohol and other substance abuse.
- Provide health education workshops and awareness campaigns on preventive health.
- Provide minimum sporting facilities and promote a sporting mindset.
- Develop mental health surveys to detect issues early and provide counselling to those who require it.
- Encourage yoga and meditation as part of mental and spiritual development.
- Plan and conduct health check-up camps in a systematic and coordinated manner.
- Create and maintain electronic health records for all students.
A comprehensive school health program is essential to ensure the health and well-being of children and adolescents. The recommendations outlined above will help to fill the gaps in existing school health programs and ensure that all students have access to the highest attainable standard of health.
Child and adolescent health are a national priority. Each child deserves access to the highest attainable standard of health without inequality. Given the above, we can conclude that the problem of adequate healthcare provision to children and adolescents is of high priority and should be taken up urgently.
The goal of any school health program is to ensure that students receive regular health checkups and are aware of healthy habits. This can be done through health promotion activities, such as promoting health literacy, personal and community hygiene, oral healthcare, better nutrition, physical activity, and menstrual hygiene management.
The program should also include health screening, preventive healthcare, and clinical assessment. This includes routine preventive check-ups, care management, and referral for students who have identified health problems. The program should also screen students for communicable and non-communicable diseases, as well as vision, hearing, oral health, nutrition, and mental health problems.
In addition to health promotion and screening, the program should also provide counselling support and first-aid training. It should also provide students with access to medicine, micronutrient supplements, and other resources, such as safe drinking water and sanitation supplies.
Here are some specific examples of health promotion activities that could be included in the program:
- Health literacy: This involves teaching students about the importance of health and how to make healthy choices.
- Personal and community hygiene: This involves teaching students about the importance of handwashing, brushing their teeth, and keeping their environment clean.
- Oral healthcare: This involves teaching students about the importance of brushing their teeth twice a day and flossing once a day.
- Better nutrition: This involves teaching students about the importance of eating a balanced diet and making healthy food choices.
- Physical activity: This involves teaching students about the importance of getting regular exercise and staying active.
- Menstrual hygiene management: This involves teaching girls about the importance of good menstrual hygiene practices.
Here are some specific examples of health screening, preventive healthcare, and clinical assessment activities that could be included in the program:
- Routine preventive check-ups: These check-ups should include a physical exam, blood pressure measurement, height and weight measurement, and vision and hearing screening.
- Care management: This involves providing students with the care they need to manage their health conditions.
- Referral: This involves referring students to other healthcare providers who can provide them with the care they need.
- Screening for communicable and non-communicable diseases: This involves screening students for diseases such as anaemia, asthma, disability, diabetes, hypertension, and mental health issues.
- Provision of first-aid and training: This involves teaching students how to provide first-aid and how to identify and respond to emergencies.
- Provision of medicine and micronutrient supplementation: This involves providing students with medicine and micronutrient supplements that they need to manage their health conditions.
- Provision of other resources and infrastructure: This involves providing students with access to safe drinking water, sanitation supplies, and sports or physical activity facilities.
The health and well-being of children and adolescents is essential for their educational outcomes and also for the future of the country. School health programs can play a critical role in improving the health of children and adolescents, and there is a strong rationale for their implementation. School health programs can provide several benefits, including:
- Improved health outcomes for children and adolescents
- Increased coverage of healthcare services
- Economic benefits
- Increased acceptability to stakeholders
However, there are several gaps in the implementation of school health programs in India. These gaps include:
- Lack of periodic and comprehensive health check-ups
- Lack of promotion of healthy habits
- Lack of awareness programs on first aid and infectious disease prevention
- Lack of long-term programs or comprehensive approaches
There is an urgent need to address the identified deficiencies by implementing a comprehensive annual school health program. The key factors that reinforce the implementation of the program are:
- The comprehensive school health program can effectively improve health outcomes or increase coverage of healthcare services for school-age children and adolescents.
- The program will also be effective in terms of economic benefits (cost–saving, cost-benefit, and/or cost-effectiveness).
- The program is more acceptable to stakeholders, such as school-age children and adolescents, parents and caregivers, teachers, and policy-makers.
School health programs are critical for the health and well-being of children and adolescents. The government, with the help of all stakeholders, needs to take up school health programs seriously and implement a comprehensive annual school health program. This will help to improve the health of children and adolescents, providing lasting benefits not only to the individuals but to society at large.
A comprehensive school health program should be implemented to address the physical, emotional, psychosocial, and educational healthcare needs of students. The program should be well-resourced and implemented effectively.
Rationale: Comprehensive school health programs are effective in improving the health of students, increasing their acceptability, and reducing inequities. Schools are a convenient and effective way to reach children and adolescents with needed healthcare services.
Implementation Considerations: The program should include the following activities:
- Assessment and check-ups: This includes general paediatric, mental, dental/oral, eye, and hearing assessments.
- Health screening and health records: This includes tracking students’ health status and providing them with health records.
- Awareness workshops: This includes workshops on menstrual hygiene and female health, de-addiction, emotional and mental management, preventive health (both communicable and non-communicable diseases), first aid, and general health.
- Counselling as and when required: This includes providing students with counselling services as needed.
- Provision of medical supplies: This includes deworming tablets, iron tablets, sanitary pads (with incinerator), first aid kits, and safe drinking water and sanitation (to the extent required).
- Promotion of sports and physical activities: This includes promoting sports and physical activities to improve students’ health and well-being.
The program should be implemented with quality and over the long term. This means that the program should be well-resourced, have clear goals and objectives, and be implemented by trained staff.
The Annual School Health Program will include the following activities to assess and improve the health of children:
- Health Risk Assessment Survey: We will survey to assess the baseline health status of all children.
- Electronic Health Record: We will create an electronic health record for each child to track their health history and needs.
- Health Screening Camps: We will conduct health screening camps to identify potential health problems so that they can be treated early.
- Mental Health Workshops and Counseling: We will offer mental health workshops and counselling to help children cope with stress and other mental health challenges.
- Health Workshops: We will offer health workshops to teach children about healthy behaviours and how to prevent diseases.
- Provision of IFA and Albendazole Tablets: We will provide IFA and Albendazole tablets to children as part of the WIFS and NDD programs, respectively.
- Sanitary Pads and Incinerators: In select cases, we will provide sanitary pads and incinerators to help girls manage their menstrual hygiene.
- First Aid Box: We will provide a first aid box for the whole year with essential medical supplies.
- Water Purifiers, Handwash Stations, and Sports Equipment: In select cases, we will provide water purifiers, handwash stations, and sports equipment to promote healthy habits.
- Other Health-Related Requirements: We will also address any other health-related requirements that may come up at a particular school.
Annual school health programs can have several positive outcomes for students, including:
- Assess the current health status of students. This will involve surveying students to identify any health risks. The results of the survey will be used to develop targeted interventions to improve student health.
- Early detection of health issues: This can lead to prevention or early treatment, which can improve overall health and well-being.
- Better mental health: School health programs can help to identify and address mental health issues, such as anxiety and depression. This can improve students’ overall well-being and ability to learn.
- Clinical counselling: School health programs can provide clinical counselling to students who need it. This can help students to identify and address the root causes of their problems, and to develop coping mechanisms.
- Higher health awareness: School health programs can help to raise awareness of health issues among students. This can lead to healthier lifestyle choices, which can have a positive impact on health in the long term.
- Guiding students on lifestyle habits: The program will provide students with guidance on how to manage their lifestyle habits for better health. This includes topics such as nutrition, exercise, and sleep.
- Empower students to become healthy individuals. This will be achieved by conducting workshops on health awareness, healthy habits, and behavioural change. The workshops will help students to make informed choices about their health.
- Lower absenteeism: When students are healthy, they are more likely to attend school regularly. This can lead to better academic performance.
- Better learning: When students are healthy and have good mental health, they are more likely to learn effectively. This can lead to better academic outcomes.
- Provide a holistic safe and healthy environment. This will involve identifying and addressing gaps in health-related infrastructure, supplies, and services in schools.
- Making schools safer and healthier: The program will help to create a more safe and healthy environment for students by addressing issues such as bullying, violence, and substance abuse.
- Providing targeted interventions: The program will use risk profiling to identify students who are most at risk for health problems. These students will then receive targeted interventions to help them improve their health.
- Collating data at the school level: The program will collect data at the school level to track the progress of the program and to identify areas where improvement is needed.
- Creating a scalable model: The program will create a scalable model that can be used to reach more students and achieve greater impact.
Herein we outline the expected budget for the program. The budget is divided into three parts:
- Program Team Expenses: These expenses are estimated every month, as they are based on manpower costs.
- Medical Camps and Workshops Expenses: These expenses are estimated on a per-activity/per-student basis, as they will vary depending on the frequency of the activities.
- Other Provisions, Audit, and General Expenses: These expenses are estimated as a percentage of the total cost or on a lump-sum basis.
The above costs are based on discussions with doctors and various associations. The estimate of per-activity cost includes the cost of personnel, transportation, and incidental expenses such as food and support staff.
Tentative Payment Schedule: We would require a 100% commitment for funds for all students or any specific number of students or specific schools. The payment schedule would be as follows:
- Advance of 30%
- Monthly payments against monthly billing (submitted along with Social Audit Report and Fund Utilization Certificate)
The overall estimate of the cost per student for the Annual Health Program to cover 1000 to 10,000 students is provided below.
| Sr. No | No. of Student | Part 1 | Part 2 | Part 3 | Total |
| 1 | 1000 | 1,560 | 1,065 | 262.50 | 2,887.50 |
| 2 | 2000 | 780 | 1,065 | 184.50 | 2,029.50 |
| 3 | 3000 | 520 | 1,065 | 158.50 | 1,743.50 |
| 4 | 4000 | 390 | 1,065 | 145.50 | 1,600.50 |
| 5 | 5000 | 312 | 1,065 | 137.70 | 1,514.70 |
| 6 | 6000 | 260 | 1,065 | 132.50 | 1,457.50 |
| 7 | 7000 | 223 | 1,065 | 128.79 | 1,416.64 |
| 8 | 8000 | 195 | 1,065 | 126.00 | 1,386.00 |
| 9 | 9000 | 173 | 1,065 | 123.83 | 1,362.17 |
| 10 | 10000 | 156 | 1,065 | 122.10 | 1,343.10 |
Real Stories, Real Results
Hear What Our Patients Are Saying!
I am thankful to Smaarogya to help me understand how my daily habits have an impact on my health and how small changes can help me lead a better life.
Priya
My wellness consultation session with Dr Sujatha was an eye-opener. It helped me understand intake of water, food, air and the environment can have a huge impact on my physical and mental energy
Arvind
Smaarogya HRA assessment is a very useful health risk assessment tool to understand our health risks and change our lifestyle to make our health better. I have every family member of mine enrolled to get their online health assessment done.
Harish bhai
Smaarogya Health Assessment is a unique health assessment tool that captures participant members' basic vitals, daily routine, lifestyle habits, and family health history and accurately predicts the health risks. Would recommend everyone to get their assessments done regularly and consult the doctor with their report.
Dr. TKM Easwar
Diabetologist
